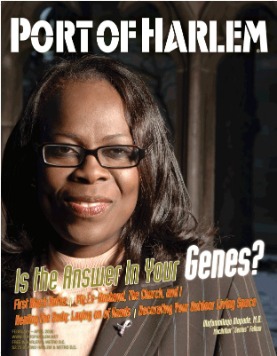
COVER CREDITS: Dr. Olufunmilayo Olopade, a John D. and Catherine T. MacArthur Foundation award winner. Photo from the University of Chicago.
20 Is the Answer in Your Genes?
How much of the health gap between Black and White Americans can researchers explain through differences in genetic make up? And what impact does the environment have on our health?
As a MacArthur Fellow, Dr. Olufunmilayo Olopade won $500,000 in unrestricted support for five years. Olopade continues to lead research efforts to understand the role our genes and environment play in the development and treatment of breast cancer in women at home and abroad.
FOCUS: Our Physical Health
14 Your Routine Physical Health
16 Healing the Body: Laying on of Hands
23 Glaucoma Takes Sight Without Warning - How to Protect Yourself
FEATURE
24 Ed Dwight – The Henry O. Flipper of Space
DEPARTMENTS
2 LETTERS TO THE EDITOR
THE PUBLISHER'S POINT
4 The U.S. Presidential Candidates: Is Any One of Them Bold Enough?
5 First Black Autos
THE OTHER SIDE
6 The Gym Cell
MIDDLE PASSAGE: A STORY OF SURVIVAL
7 My Ex-Husband, The Church and I
MONEY
8 Legal Matters that Matter to Artists, Writers and Photographers
OUR SPACE
10 Decorating Your Outdoor Living Space
TRAVELSTORY
12 The “D”
RECIPE
25 Under-the-Sea Cakes
BOOK REVIEW
26 No Safe Place: A Gen-X Childhood in Black
COMING UP
27 Mid-Atlantic Quilt Festival, The Color Purple, Freda Payne and more.
ENTERTAINMENT
28 Home to Harlem
Also in 2005, BiDil became the first drug the United States government approved specifically for Black people. Meanwhile, researchers in suburban Chicago concluded that high rates of hypertension among African-Americans might have more to do with lifestyle than race.
Using race in the practice of medicine often reinforces old prejudices about biological differences among socially-defined people or that scientifically defined races even exist - - concepts that University of Maryland medical anthropologist Fatima Jackson finds ludicrous. “Race is a sociological and cultural construct and is far too ambiguous biologically to be genetic. In other words, you will not find a single genetic trait within a so-called "race" that is found 100% within the "race" and 0% outside of the "race,” Jackson says.
Black women are less likely to get breast cancer than White women, but are more likely to get the disease when they are young and are much more likely to die from it. These facts puzzled Olopade and led to her groundbreaking Pan-African study.
While using race as a medical tool remains controversial, Olopade says that the medically important issue is not race itself but the predisposing genes that follow racial patterns. The most difficult questions adds Olopade is how much of the "answer" is in the genes and how much is in the environment. “Most diseases have both genetic and environmental components, and of course the genes and the environment interact with each other in complicated ways; for instance, certain kinds of stress may activate certain genes. This is something that we need to understand for breast cancer and for all complex disorders,” she continued.
ER-negative Breast Cancer Tumors - A Middle Passage Survivor
Black women are less likely to get breast cancer than White women, but are more likely to get the disease when they are young and are much more likely to die from it. These facts puzzled Olopade and led to her groundbreaking Pan-African study.
Her discovery started on one of her biennial vacations to her birth country, Nigeria. In 1997, she began working with breast surgeon Dr. Adebarnowo at the University of Ibadan, her alma mater, by collecting and studying data on Nigerian women with breast cancer. (Olopade is continuing the study in the United States to further document the link between Black women at home and abroad.) The Nigerian study led to three crucial findings:
1. Tumors in African women are more likely to develop from a different set of cells in the
breast that can turn into a more aggressive type of breast cancer.
2. Breasts tumors in African women are less likely to express a genetic marker that the breast
cancer drug Herceptin attacks.
3. Eight in ten tumors in African women are estrogen receptor negative (ER-negative). This
rendered the anti-cancer drugs that target female hormones within breast cancers useless.
“These ER-negative tumors are not sensitive to the female hormone estrogen and thus do respond to drugs, such as tamoxifen, that work by keeping the estrogen from reaching cancerous cells and stimulating growth. Because ER-negative breast cancer moves fast, physicians must catch it early. Without chemotherapy treatments most patients die within two years,” warns Olopade.
Research also shows that in Africa most breast-cancer cases occur around age 40, as opposed to the late 50s or 60s in the U.S. Most U.S. screening guidelines, based primarily on Caucasian data, recommend an annual mammogram beginning at 50. However, African Americans are more like their genetically related Continental sisters and are likely to get the disease between ages 40 and 50. “Black women,” Olopade says, “should first get screened around age 25, and those who are high-risk, for example, women with a family history of the disease - - even younger.”
BiDil - “The Black Drug?”
However, Jackson warns: “Don't believe the hype!” Since many who society identifies as White carry some of the same genes that Blacks carry, she says, “I am positive that many European Americans with cardiovascular disease (diseases that involve the heart or blood vessels) would benefit from the pharmaceutical components that make up Bidil.”
Hypertension and Oppression
For many years people assumed that genetics and psychosocial factors, like the affects of surviving oppression, predisposed African-Americans to high blood pressure. However, many came to this conclusion without looking at high blood pressure data for international Black populations.In 2005 Dr. Richard Cooper led researchers in a study that compared blood pressure of Black populations in Nigeria, Jamaica, and the United States, and Whites in the United States, Canada and five European countries. While Blacks and Whites share a common genetic ancestry with those of the same “race,” living in various countries “they live under very different social and economic conditions,” says Cooper.
When viewed internationally, there is a wide variation of high blood pressure between Blacks and Whites. Cooper’s results show hypertension in people of African origin ranging from 14 to 44 percent, while in European populations it ranges from 27 to 55 percent.
Though “Blacks are less likely to have an allergic reaction,” explained Port of Harlem contributor Dr. Theo Hodge, Jr., “doctors should not depend upon race alone to determine whether to prescribe the medication.”
The study revealed Blacks in Nigeria have a hypertension rate that is more than half the rate of White Europeans and White Americans. Results also show the incidence of high blood pressure among Blacks seem to increase with industrialization. The total prevalence of hypertension in Nigerians ages 35 to 64 is 13.5 percent, in Jamaicans it is 28.6 percent, and in U.S. Blacks, it is 44 percent. The study, says Cooper, “concluded that high rates of hypertension might have more to do with lifestyle than with racial origin.”
Genetic Testing and HIV Management
Abacavir,a medication that doctors use to treat HIV, causes potentially life threatening allergic reactions in 2 to 9 percent of patients. Though “Blacks are less likely to have an allergic reaction,” explained Port of Harlem contributor Dr. Theo Hodge, Jr., “doctors should not depend upon race alone to determine whether to prescribe the medication.”
Studies show that patients who are allergic to Abacavir often posses within their genetic maps an area known as HLA-B*5701. Echoing Jackson’s concerns about equating race with genetics Hodge continued, “assumptions that a Black patient will not react to Abacavir are unacceptable. A blood test is now available to assess if this genetic area exists in individual patients.”
Looking Toward the Future
The question remains: How much of the health gap between Black and White Americans can researchers explain through differences in genetic make up? And what impact does the environment have on our health? Jackson, who specializes in biological anthropology says, “In world history, the gene-environment interactions are consistently much more important than the naked genetics alone.”